UPDATE: I didn’t expect malpractice reform to come out of the House but I didn’t expect a poison pill for tort reform either.
Well, buried in the 1,990 pages of the House health-care bill that was released on Thursday by Pelosi is a provision in Section 2531 that provides incentive payments to states that provide “an alternative medical liability law” that prevents or prompts “fair resolution” of disputes. However, no such incentive will be paid to any state that limits “attorneys’ fees or impose caps on damages.”
Thus, California’s 34 year old cap on non-economic damages in MICRA would preclude it receiving any incentive payment, what ever that is.
The Pelosi bill has now been dumped on the House and is due to be voted on in a little more than a week. It is insanely expensive. The The CBO score is even hedged by doubts.
Those longer-term projections assume that the provisions of H.R. 3962 are enacted and remain unchanged throughout the next two decades, which is often not the case for major legislation. For example, the “sustainable growth rate” mechanism governing Medicare’s payments to physicians has frequently been modified to avoid reductions in those payments, and legislation to do so again is currently under consideration in the Congress. The bill would put into effect (or leave in effect) a number of procedures that might be difficult to maintain over a long period of time. It would leave in place the 21 percent reduction in the payment rates for physicians currently scheduled for 2010. At the same time, the bill includes a number of provisions that would constrain payment rates for other providers of Medicare services. In particular, increases in payment rates for many providers would be held below the rate of inflation (in expectation of ongoing productivity improvements in the delivery of health care).
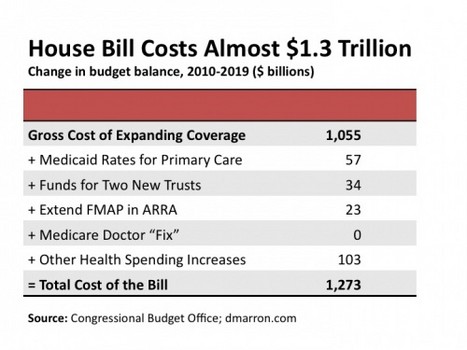
It contains a number of bad ideas and one lie. First the lie. In 1997, Congress passed a law that said Medicare costs had to remain within the CPI or they would cut doctors’ reimbursement. It didn’t and they didn’t. Every year, Congress would pass a bill that suspended the rule for one year. By now, the cuts in doctor reimbursement, if implemented, would be about 25%. Harry Reid tried to pass a separate “doc fix” bill last week in the Senate and it didn’t pass. The idea was to reverse the 25% cut in reimbursement but keep it out of the Finance Committee bill to keep the CBO estimate below a trillion dollars.
At issue was the sustainable growth rate, a Medicare formula that’s called for physician payment cuts in almost every year of the last decade, threatening seniors’ access to care and leaving Congress to step in with temporary fixes — effectively kicking the can down the road. Sponsored by Sen. Debbie Stabenow (D-Mich.), the bill would have eliminated the formula once and for all, allowing Congress to establish a new method of updating doctor payments that better reflects the cost of treating Medicare patients.
“This is about strengthening and protecting Medicare,” Stabenow said just before the vote.
Wednesday’s vote means that Democrats will have to find another way to prevent a 21.5 percent pay cut from hitting Medicare doctors next year, likely with a temporary patch that will eliminate the cut but keep the formula in place. The Senate Finance Committee bill includes a one-year band-aid, at a cost of just under $11 billion.
Why is this a problem ?
Medicare reimburses physicians substantially less than private insurers. Medicare pays hospitals and doctors, respectively, 71 percent and 81 percent of private rates. For doctors seeing Medicare patients, this is often barely enough to break even. For hospitals, the Medicare payments don’t even cover the cost of seeing patients — meaning that hospitals actually lose money on Medicare patients. The sheer size of the federal government essentially transforms negotiations into “a take it or leave it” proposition that allows Medicare to get away with such stinginess. Providers would be better off negotiating with the mafia.
Actually, the Medicare reimbursement varies by specialty, being better for primary care and worse for specialties that are expensive. Some areas get about 20% of charges. That is down from 80% or more 30 years ago.
The House bill puts the cost of the “doc fix” at zero. Just one more lie.
Another bad idea is extending Medicaid eligibility to 150% of the poverty level. Few doctors accept Medicaid now anyway. More and more are dropping Medicare. What else is in there ?
How about loans for veterinary students ?
Fun Fact: Page 1255 of the bill makes veterinary students eligible for federal grant funding, including scholarships and loan forgiveness. There is $283 million in spending authorized under these sections – meaning we could be spending hundreds of millions to pay for veterinarians while we have a deficit of over $1 trillion.
For a clue about why this is in there:
“Division C” of a “comprehensive” reform of the health-care system should at least be skimmed. This section, starting on page 1209, called “Public Health and Workforce Development,” contains a hodgepodge of new programs, and reauthorizations and amendments to existing programs, each of which has a fairly direct line to some interest group that wants something from the federal trough. Many are just one step up from an appropriations earmark as examples of pork.
It goes on for 427 pages.
What would I do ? I’ve spent some time explaining what I think would be a good approach. I base a lot of this on the French System. It has had its problems but most of those stem from France’s economic problems. As Obama and the Democrats take us down the road to socialism, we will have similar problems with sluggish economy and government debt.
I’ve seen a couple of articles advocating some of these ideas but they can get too libertarian. For example, catastrophic insurance is the basis for any sensible system. Health savings accounts should be an important part of a reform but there are problems. Our present system has badly distorted the price of medical services. Both Medicare and private insurance have gone heavily to the concept of “discounts” in medical prices, both hospital prices and doctors’ fees. That is where $50 aspirin tablets come from. In the days of Blue Cross and when costs were not the issue, nobody cared about hospital prices. Blue Cross was a system that was based on the annual operating costs of hospitals. Individual items of service were not billed as such. It was not important to figure out how much the emergency department made or lost each month. The ICU didn’t even exist until the 1950s. Cash services like obstetrics were loss leaders. The prices were low because the hospital wanted that young family to get used to coming there for care. Ditto with the ER. Neither was expected to make money and nobody really did cash accounting to figure out what they cost.
The insurance companies started it. The commercial insurers, who had much of the industrial and union business, wanted prices. They were tired of paying what they feared were inflated daily room rate charges. Hospitals had no idea what these services cost them. To this day, hospitals are incredibly inefficient. The result was a crazy quilt of billed charges, many of which had nothing to do with costs. A second result has been intense pressure to reduce hospital stay. As a result, the daily charges have skyrocketed. Why ? The costs of a hospital admission are almost all incurred on one day, the surgery day or the day of admission when all the tests are done. If the hospital stay is five days, as was common 40 years ago, the costs get spread over all five days. Now, they are all packed into one day. The Europeans think we are crazy with the obsession to shorten length of stay. They are correct but here is no convincing Medicare or insurance companies. Same day admissions (also called AM Admits) for surgery began in the 80s and make no sense. It used to be that a patient for elective surgery came in the afternoon before, the prep and tests were done, and the patient got a good night’s sleep. Now, the patient gets up at 3 AM to come to the hospital, extra staff have to be present early in the morning and the risk of error is far higher. The cost, I’m sure, is about the same.
Anyway, the cash prices are so distorted that the HSA is almost useless unless the claim is processed through the insurance company.
Secondly, many older people will have a hard time paying for care if they haven’t been saving in their HSA for 20 years and they haven’t. There has to be a transition. My ideas about the French system would apply here.
I don’t know if these bills will actually pass. If they do, the taxes and regulation will dominate the first few years and I am not sure that we will not see another catastrophic care fiasco. I don’t know how it will end. Hopefully with nothing.